A comprehensive quality assurance program has the potential to directly contribute to better patient outcomes. It’s vital to know how to perform Ultrasound Probe Quality Assurance inspections.
Regular testing provides a mechanism to monitor probe performance and correct as needed. The end result is a continuous quality improvement program that ensures optimal diagnostic outcomes.
As vital as it is to perform regular testing, there is no one standardized process or criteria for effectively field-testing ultrasound probes in the industry.
Innovatus Imaging has designed a guide to assist technicians with understanding industry standard testing criteria for assessing probe performance. The guide presents background information on probe design, detailed testing methods, root cause analysis and troubleshooting techniques.
This guide is also available as a pdf. Request your copy below.
WHAT YOU’LL LEARN
- Key terminology
- Overview of the components and technologies used in modern probes
- Common quality assurance tests from the most popular accreditation boards including: – American College of Radiology (ACR) – American Institute of Ultrasound in Medicine (AIUM)
- Best practices and ground rules for performing image quality testing
- Common testing methods, pass/fail criteria and techniques for troubleshooting image quality problems
- How to assess probe performance in the field
- How to acquire and assemble the quality control data required for accreditation
Contents
Industry Standards
Key Terminology
Best Practices
How to Perform Field-based Transducer Testing
- ImageUniformity
- Maximum Depth of Penetration and Functional Resolution
- Geometric Accuracy
- Spatial Resolution
- Contrast Resolution
- Cable Noise Test
- Electro-Mechanical Functionality
Documentation Template
Industry Standards
With more than 300 diagnostic ultrasound transducer models on the market at any one time, criteria and methods for testing image quality testing can be confusing.
The physical and technical design of one transducer can greatly vary from one model to the next. Without a firm knowledge base, consistent methodology and well-defined pass/fail criteria, test results can be highly variable and inconsistent.
Standards established by several accreditation boards offer a framework for testing and solid criteria for assessing the performance of devices used within diagnostic ultrasound.
The two primary accreditation boards
- American College of Radiology (ACR)
- American Institute of Ultrasound in Medicine (AIUM)
Common requirements for accreditation
- Case study submissions
- Personnel education and continued training
- Document storage and record-keeping
- Policies and procedures to safeguard patients, ultrasound personnel and equipment
Common functional tests for accreditation
- Image uniformity
- Maximum depth of penetration
- Geometric accuracy
- Spatial accuracy
- Contrast resolution
Tests for cable noise and electro-mechanical functionality are not addressed by these boards, but offer a more comprehensive performance assessment.To help close the industry’s training gap, Innovatus Imaging has established a set of guidelines that will help you perform consistent ultrasound transducer quality assurance assessments. The goals are to build technical confidence and to minimize variability so that clinician scan trust the tools that they rely upon the most to provide the most accurate diagnosis possible.
Key Terminology
Each component within the transducer plays a vital role in the overall performance of the device.
It’s critical to understand the purposes and the functions associated with basic transducer construction prior to presenting best practices for assessing performance.
A failure in one area of the transducer may affect the performance of or the results provided by another.
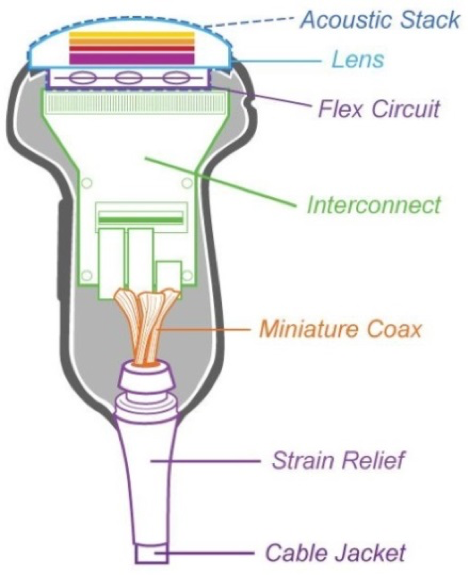
Lens
- Mechanical focus of ultrasound beam
- Model-specific materials and dimensioning
- Electrical insulation
- Fluid barrier
- Single or multilayer materials, must be ISO 10993 compliant
Matching layer(s)
- Maximizes transmission of energy from acoustic array to tissue by reducing reflection and increases spectrum of frequencies(bandwidth) emitted by transducer
- Consists of one to seven different layers based on transducer model
- Generally ¼ wavelength of the array’s center frequency in thickness
Acoustic Array
- Converts electrical energy to mechanical energy (pressure wave) and vice versa
- Consists of several to thousands of individual elements
Shielding
- Reduces the effects of electromagnetic interference
- Typically surrounds the array, the backing material and scan head electronics
Backing material
- Dampens crystal vibrations to reduce pulse duration, which increases axial resolution
Flex circuit
- Flexible circuit board that connects the inter connect board to the individual elements
Interconnect/Scanhead electronics
- Bridge between individual coaxial cables and flex circuit
- May include multiplexing circuitry, as well as beam forming circuitry
Miniature coax
- Bridge between the connector electronics and the scan head electronics
- Internal signal wire enclosed within a braided shield
- Typically the diameter of a hair
- Model-specific length, impedance and capacitance
Strain relief
- Reduces stress on main and coaxial cables
Cable jacket
- Protects main transducer cable
Main cable
- Contains several to hundreds of individual coaxial wires
- Model specific shielding to minimize the effects of electromagnetic interference
Best Practices
Ultrasound Probe Quality Assurance testing on transducers is a key contributor to improving the accuracy of patient diagnoses, treatment plans and ultimately patient outcomes.
Routine – and consistent – testing is vital to ensuring that devices are performing at a level very similar to that when they were purchased.
By following these best practices, you’ll be able to feel confident in equipment quality. The following can be considered a baseline for beginning the QA process.
System and environment
- Ensure a quality equipment ground.
- Clean the scanner’s transducer ports.
- Disconnect all transducers except the one being tested.
- Disconnect the network cable from the rear of the scanner.
- Adjust room lighting to typical scanning room intensity.
- Display brightness and contrast:
- Use the system grayscale bar to adjust brightness so the darkest shade of gray is barely visible.
- Assure that the grayscale bars are graduated or stepped.
- Contrast is adjusted for “white whites” but not blooming.
- Confirm any recommendations or adjustments with the sonographer.
Testing devices
- A tissue-mimicking phantom MUST be used to properly assess image quality.
- The same model and type of phantom should be used between each assessment.
- Suppliers include Gammex and ATS.
- Do not attempt to assess image quality viewing a patient scan.
- Although nice to have, specialized high-tech testing devices are not needed to assess transducer performance in the clinical setting.
Consistency between testing is key
- Tests should be conducted always using identical system settings and presets.
Example: Every Philips C5-1 should be tested using the same preset.
Suggested presets
Linear probes Vascular preset
Curved probes Abdominal preset
Endo-cavity OB present
Sector Cardiac preset
- The number of focal points should be minimal, only one to two.
- Turn off all options such as harmonic imaging, spatial compounding and image smoothing (these options may mask transducer and scanner deficiencies).
Brand specifications
Philips THI, SonoCT and xRes
Siemens THI, MultiHz and SieClear
GE Octave, Crossbeam and CHI
- Periodic inspections should occur at original equipment manufacturer recommended intervals, if not more often. (Accreditation boards recommend at least annually.)
Acceptance testing should be performed when:
- Equipment is new and is being installed
- Equipment has been in storage and is being returned to service
- Image-related assemblies, including transducers, have been repaired or replaced
Visual inspections should be conducted by sonographers daily
- By addressing minor physical deficiencies, prior to them progressing to a point where they impact image quality, long-term service costs can be minimized.
- Inspect components for the following concerns:
Lens Holes, cuts, missing sealant, bulges, air bubbles, separation in materials
Housing Cracks, separation, missing sealant, sharp edges
Strain reliefs Separation from housing, cuts, holes, excessive stiffness
Cable Cuts, holes, exposed wiring, roll-over damage, excessive stiffness
Connector Deformations, cracks, missing/malfunctioning hardware
Pin-bank Bent pins, corrosion, burn marks, excessive dust/debris
How to Perform Field-based Transducer Testing
The following are instructions on how to conduct common functional tests required for accreditation.
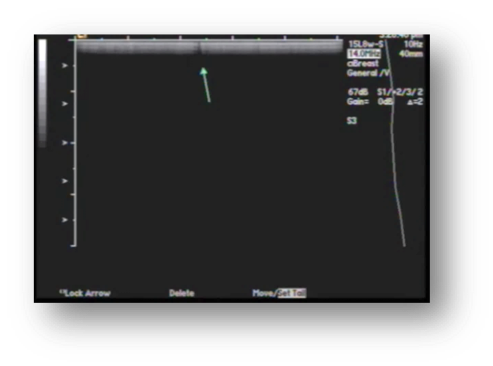
Image Uniformity
Common names
Element testing, channel testing
Purpose
To perform element-to-element or channel-to-channel comparison
Region of interest
The entire width of image
Scanner settings
Frequency Highest possible
Depth 3-6 cm of depth
Focus Single focal point located in the very near field
Gain Adjust overall gain and TGC so that mid-range gray level exists over the entire image
Recommended testing method
- Adjust the depth to 3-6 cm (this is probe dependent)
- Adjust the number of focal points to one (or the focal zone to the smallest possible size)
- Adjust the focal zone to the top-most position of the image
- Adjust the TGCs so that the background is as uniform as possible and is shaded in the middle-range of the grayscale
- Slowly move the probe back and forth along the phantom’s surface and monitor the image on the display for any vertical non-uniformity (weak elements – minor dropout – will be easier to visualize when the probe is in motion)
Visual criteria
Use the following information to determine next steps for service:
Fine shadow on a single channel: Minor flaw
Multiple fine shadows or wide shadow on multiple channels or elements : Major flaw
Ranking and action levels
| Ranking | Visual criteria | Potential impact | Action |
| 1 | No flaws are present | Operating as expected | No action required |
| 2 | One or two minor flaws are present | Considered operational and can be used for scanning | Inspect occasionally for possible additional deterioration over time |
| 3 | Three or more minor flaws are present | Borderline based upon location | Replace as soon as convenient |
| 4 | Major flaws are present | Unacceptable for clinical use | Remove from service immediately |
Potential root causes for the artifact
| Probe | Root cause/Troubleshooting |
| Acoustic lens | Lens delamination: wide shadowing |
| Acoustic array | A single or multiple missing or weak elements may show small artifacts |
| Cable/wiring harness | Test for intermittencies |
| Pins/connector | Inspect regularly: clean dust from pinned connectors, clean pin-less connector interfaces |
| System | Root cause/Troubleshooting |
| Connector board | Inspect regularly: Examine for damaged pins. Clean dust from scanner ports. Test the probe on multiple ports. |
| Front-end board | Test the probe on another scanner to rule-out a probe/connector issue. |
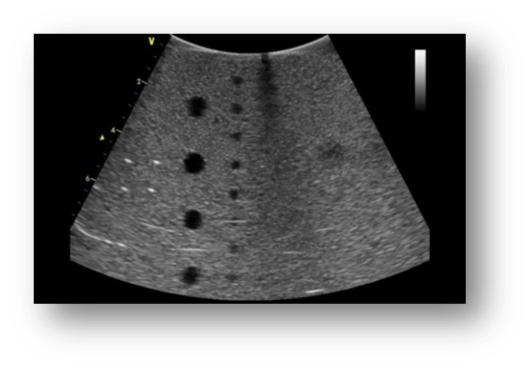
MaximumDepth of Penetration and Functional Resolution
Common names
Maximum visualization, relative penetration or functional resolution
Purpose
To provide an indication of overall sensitivity of a scanner/transducer to detect weak signals
Regions of interest
Fiber targets Maximum depth
Anechoic targets Functional resolution
Scanner settings
You must use same preset for each individual probe model and same model phantom.
Frequency Typical for the probe model
Depth Probe dependent
Focus Adjusted to meet needs
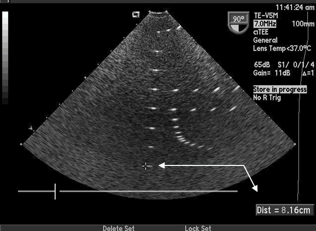
Maximum Depth of Penetration
The maximum distance between the top of the image and the deepest vertical target that can be visualized
Recommended testing method
- Position the transducer over the vertical group of line targets until a clear image is obtained
- Adjust the depth to a point no deeper than needed to display as many vertical targets as possible
- This will be different for each make and model of probe
- Adjust the focal zone to match the depth of the deepest visible target
- Utilize cursors to measure the distance between the top of the phantom and the deepest target that can be clearly imaged
This distance should remain consistent over the life of the probe

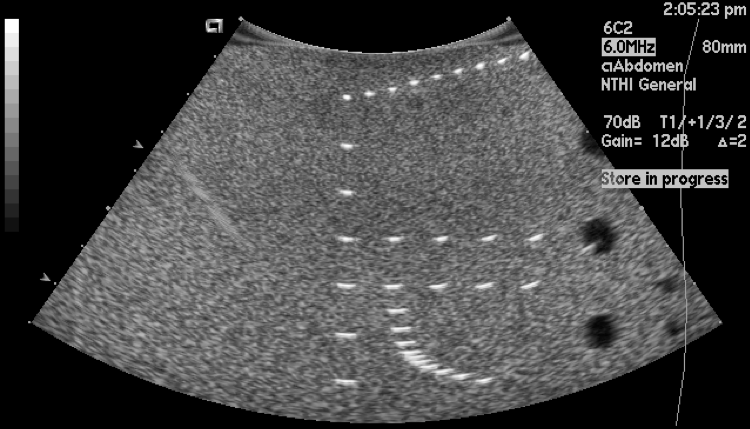
Functional Resolution
The maximum distance between the top of the image and the deepest and smallest anechoic target that can be visualized.
Recommended testing method
- Position the transducer over the anechoic target structures until a clear image is obtained
- The actual depth will depend on the specific make and model of the probe
- Adjust the focal zone to match the depth of the smallest anechoic target that is clearly visible
- Examine the image and determine the depth of the smallest anechoic target that is clearly visible
This distance should remain consistent over the life of the probe


Ranking and action levels
- A 5% decrease in maximum depth of penetration(from the first measurement) is cause of concern
- A 10% decrease is cause for corrective action to the probe or scanner
Potential root causes for a change
| Probe | Root cause |
| Acoustic lens | Lens thickness: improper repair |
| Fluid/gel infiltration | |
| Damage to matching layers | |
| Acoustic array | Arrays can degrade over time (>8-10 years) |
| System | Root cause/Troubleshooting |
| System | Inconsistent preset |
| Display settings |
| Environmental | Root cause/Troubleshooting |
| Environmental | Ambient lighting |
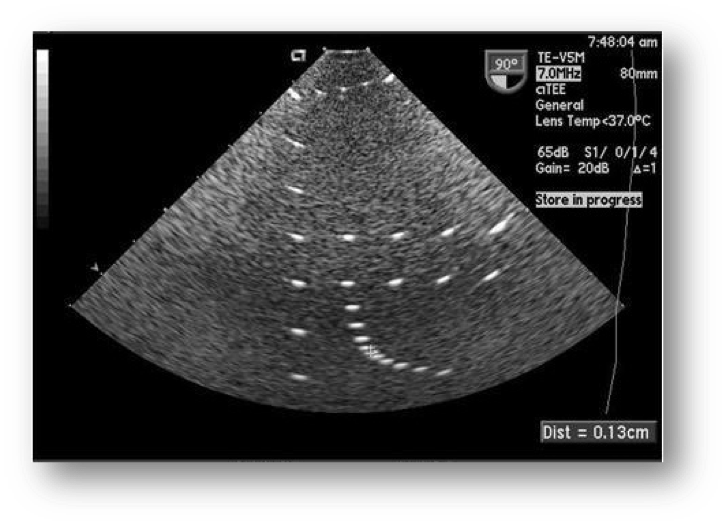
Geometric Accuracy
Common names
Measurement accuracy
Purpose
To verify both horizontal and vertical accuracy
Region of interest
Respective target groups
Scanner settings
Frequency Typical for the probe model
Depth Probe dependent
Focus Single focal point located in the center of the area to be measured
Vertical measurement
- Position the probe above the column of reflector targets in the center of the image
- Choose two targets separated by a distance that is consistent with the type of transducer
- Place cursors in the middle of each target
Verify that the target distance is with 1.5% or 1.5mm (whichever is greater)
Horizontal measurement
- Choose two targets that are separated by a distance of at least half of the image width
- Place cursors in the middle of each target
Verify that the target distance is within 2% or 2mm (whichever is greater)

Potential root causes for inaccuracies
| Probe | Root cause/Troubleshooting |
| Acoustic lens | Lens thickness, lens material: improper repair |
| Compare measurements between multiple probes of the same model |
| System | Root cause/Troubleshooting |
| System | Gross inaccuracies may indicate a major system issue |
| Compare measurements between multiple systems of the same model |
Spatial Resolution
Common names
Axial/lateral resolution
Purpose
To verify the minimum distance at which two targets can be individually visualized
Region of interest
Resolution targets
Scanner settings
Frequency Typical for the probe model
Depth Phantom dependent
Focus Single focal point located in the center of the area to be measured
Lateral resolution (X)
- Ability to distinguish between two objects perpendicular to ultrasound beam
- Varies with depth and focal point(s)
Axial resolution (Y)
- Ability to distinguish between two objects parallel to ultrasound beam
- Does not vary with depth
Elevational resolution (Z)
- Ability to distinguish between two objects perpendicular to scan plane (slice thickness)
- Varies with depth
Recommended testing method
- Position the transducer over the axial-lateral resolution group
- Adjust the focal zone to the center (or just above the center of the targets)
- Examine the image and determine the distance at which the targets are clearly displayed as separate target points
The distance should remain consistent over the life of the probe
Potential root causes for changes
| Probe | Root cause/Troubleshooting |
| Acoustic lens | Lens delamination |
| Lens thickness, lens material: improper repair | |
| Compare measurements between multiple probes of the same model |
| System | Root cause/Troubleshooting |
| System | Improper focal point location |
| Gross inaccuracies may indicate a major system issue | |
| Compare measurements between multiple systems of the same model |
Contrast Resolution
Common names
Gray scale, gray scale resolution
Purpose
To provide an indication of the system’s and the probe’s ability to distinguish between objects of similar and varying densities
Region of interest
Gray scale targets
Scanner settings
Frequency Typical for the probe model
Depth Dependent upon phantom model
Focus Positioned at or right-above targets
Gain Adjust overall gain and TGC so that mid-range gray level exists over the entire image.
Recommended testing method
- Position the transducer over the gray scale target group until a clear image is obtained
- Adjust the focal zone to the center or just above the center of the target
- Examine the image
- All shades of gray should be clearly visualized (background and targets).
The targets should appear circular in shape and vary in the degree of brightness ranging from low to high levels of contrast

| Probe | Root cause/Troubleshooting |
| Acoustic lens | Lens thickness: improper repair |
| Fluid/gel infiltration | |
| Damage to matching layers | |
| Compare results between multiple probes of the same model | |
| Acoustic array | Arrays can degrade over time (>8-10 years) |
| System | Root cause/Troubleshooting |
| System | Inconsistent preset |
| Display settings |
| Environmental | Root cause/Troubleshooting |
| Environmental | Ambient lighting |
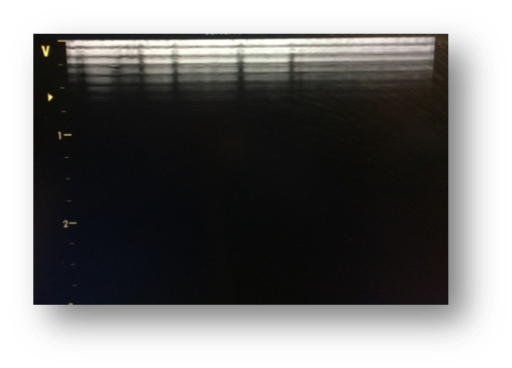
Cable Noise Test
Purpose
To identify intermittencies and breakdowns in signal wiring in the cable harness
Region of interest
Entire width of image
Scanner settings
Frequency Typical for the probe model
Depth 6-8 cm
Cardiac probes CW Doppler mode
Non-cardiac probes Color Doppler mode
Recommended testing method: cardiac probes
- Assure that the lens is clean and dry
- Enable CW Mode
- Adjust the volume to an acceptable level
- Use the trackball to move the cursor line slightly left or right of center
- Avoid a straight vertical line
- Flex each strain relief looking and listening for unacceptable noise
- Move the cursor line to several other locations and evaluate the noise level
- If cable has roll-over damage, flex/stress the damaged region
Recommended testing method: non-cardiac
- Assure that the lens is clean and dry
- Enable color Doppler mode
- Size and position the color box to span the entire width of the image
- Depth of color box should span less than 5 cm
- Adjust the color gain so that there is only very minor speckling in the image
- Flex each strain relief looking for streaks off lashing color
- If cable has roll-over damage, flex/stress the damaged region
Potential root causes for artifact
| Probe | Root cause/Troubleshooting |
| Wiring harness | Intermittent wiring: Heavy static sounds in CW mode, streaks of flashing color in color mode |
| Major wiring damage: intermittent dropout in the 2D imaging |
Electro-mechanical Functionality
Purpose
To identify electro-mechanical failures in 3D/4D volumetric probes
Region of interest
Probe only
- Internal electro-mechanics
- Motor
- Sensor
Scanner settings
Mode 3D/4D
Recommended testing method
- Visually inspect the dome for abrasions and signs of impact
- Enable continuous 3D/4D acquisition
- Apply slight pressure to dome
- An error message should not be displayed
- Stress strain reliefs and any area on the cable that shows evidence of roll-over damage or pinching.
Potential root cause of failure
| Probe | Root cause/Troubleshooting |
| Probe | Impact to dome: internal electro-mechanical damage |
| Motor failure | |
| Sensor failure |
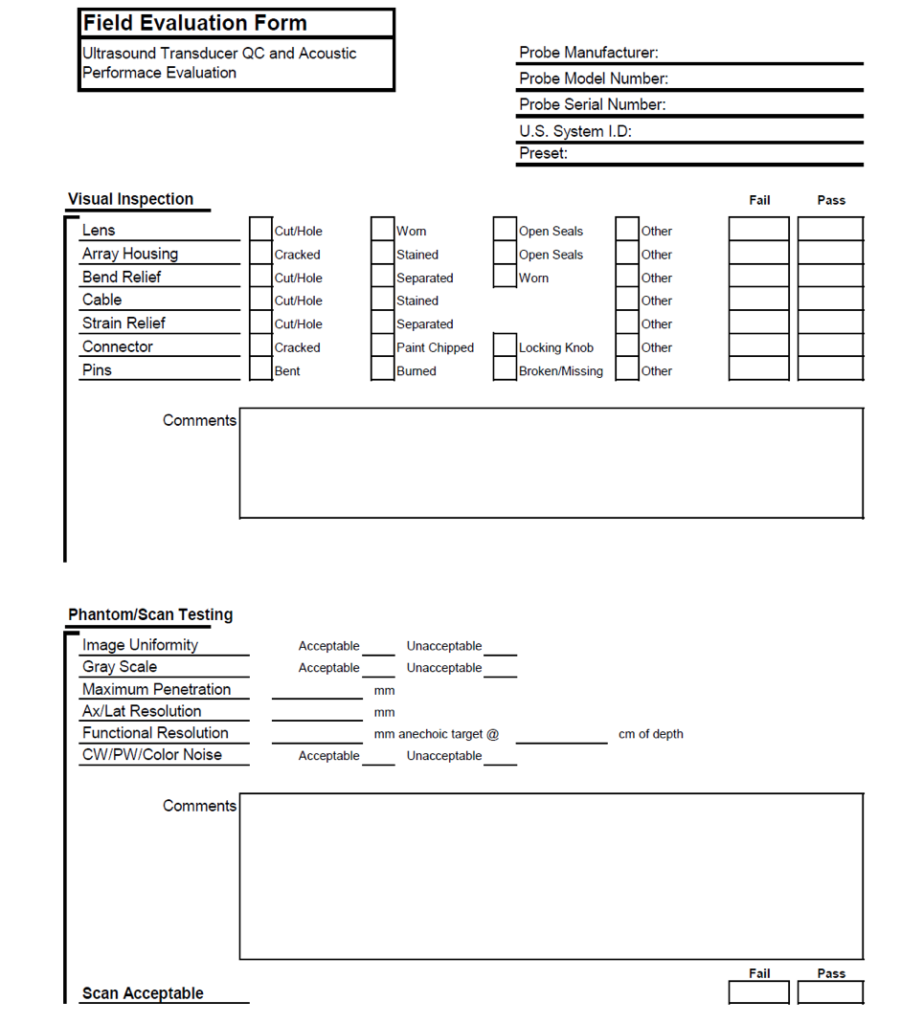
DocumentationTemplate
Currently, there is no standardized form within the industry for documenting Ultrasound Probe Quality Assurance or system performance. Below is an example of a form which can be created using Microsoft Excel. Our team can help to customize a form to meet your needs.

Comments 3
I have a question regarding on how to take the geometry accuracy measurement or a true distance in Axial and lateral my question how do you take the reading. If you can help me on that I appreciate it.
I would like a copy of this guide.
Good information for people just getting into field.